Parenteral nutrition, often referred to as PN, is a method of providing essential nutrients directly into the bloodstream when a person is unable to eat or digest food properly. It’s like giving your body a direct infusion of nutrients, bypassing the digestive system altogether. This method is typically used when a patient’s gastrointestinal tract is unable to absorb nutrients adequately, such as in cases of severe illness, surgery, or medical conditions that affect digestion.
Understanding Parenteral Nutrition
Imagine your body as a machine that needs fuel to function properly. Normally, we get our fuel from the food we eat, which is broken down in the digestive system and absorbed into the bloodstream. However, when the digestive system isn’t working correctly, the body may struggle to get the nutrients it needs to stay healthy and function optimally. That’s where parenteral nutrition comes in.
How It Works
Parenteral nutrition involves delivering a carefully balanced mixture of nutrients directly into the bloodstream through a vein, usually in the arm or chest. This mixture typically includes carbohydrates, proteins, fats, vitamins, minerals, and electrolytes, providing the body with everything it needs to maintain energy, repair tissues, and support vital functions.
Indications for Use
Parenteral nutrition may be prescribed for various medical conditions, including:
- Severe malnutrition
- Gastrointestinal disorders
- Short bowel syndrome
- Inflammatory bowel disease
- Cancer treatment side effects
- Bowel obstruction or fistula
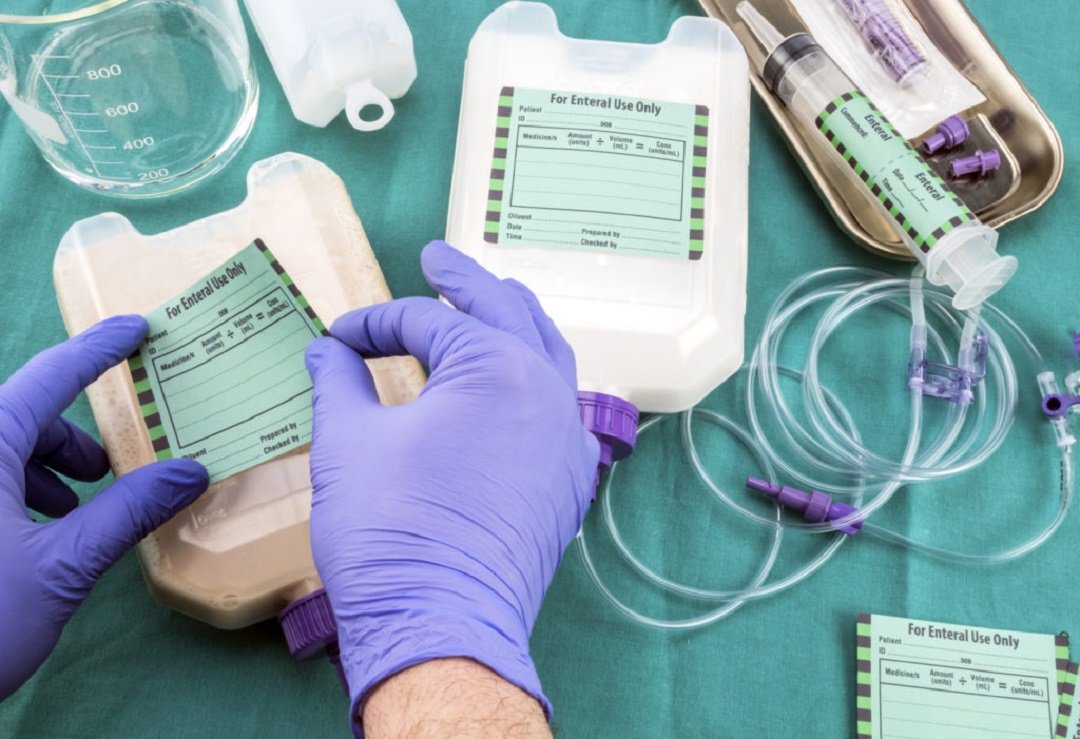
Components of Parenteral Nutrition
Think of parenteral nutrition as a customized cocktail of nutrients tailored to meet an individual’s specific needs. Here’s what typically goes into the mix:
- Carbohydrates: Provide energy for cellular functions and fuel the body’s metabolic processes.
- Proteins: Essential for tissue repair, muscle maintenance, and immune function.
- Fats: Serve as a concentrated source of energy and aid in the absorption of fat-soluble vitamins.
- Vitamins and Minerals: Ensure proper functioning of biochemical pathways and support overall health.
- Electrolytes: Maintain fluid balance, regulate nerve and muscle function, and support cardiovascular health.
Administration of Parenteral Nutrition
Administering parenteral nutrition requires specialized equipment and careful monitoring to prevent complications. Here’s how it’s typically done:
- Central Venous Catheter: A catheter is inserted into a large vein, such as the subclavian vein or jugular vein, to deliver the nutrient solution directly into the bloodstream.
- Continuous Infusion: The nutrient solution is infused slowly and continuously over a 24-hour period to ensure a steady supply of nutrients.
- Monitoring: Patients receiving parenteral nutrition require regular monitoring of vital signs, fluid balance, electrolyte levels, blood glucose, and liver function to prevent complications such as infections, electrolyte imbalances, and liver dysfunction.
FAQs (Frequently Asked Questions)
Who needs parenteral nutrition?
Parenteral nutrition is typically prescribed for individuals who cannot meet their nutritional needs through oral or enteral feeding due to medical conditions affecting the gastrointestinal tract or inability to tolerate food orally.
Is parenteral nutrition safe?
While parenteral nutrition can be lifesaving for patients with severe malnutrition or gastrointestinal disorders, it carries risks of complications such as infections, metabolic abnormalities, and catheter-related complications. Close monitoring by healthcare professionals is essential to minimize risks and ensure optimal outcomes.
How long can someone be on parenteral nutrition?
The duration of parenteral nutrition therapy varies depending on the underlying medical condition and the individual’s response to treatment. Some patients may require short-term parenteral nutrition support during acute illness or surgery. While others may need long-term or even lifelong therapy for chronic conditions.
Can parenteral nutrition be administered at home?
Yes, with proper training and supervision, some patients can receive parenteral nutrition therapy at home. Home parenteral nutrition programs allow patients to maintain independence. And quality of life while receiving the nutrients they need to support their health.
What are the alternatives to parenteral nutrition?
In some cases, enteral nutrition, which involves delivering nutrients directly into the gastrointestinal tract through a feeding tube, may be a viable alternative to parenteral nutrition. However, enteral nutrition may not be feasible or sufficient for patients with severe malabsorption or intestinal failure.
In conclusion, parenteral nutrition is a crucial medical intervention that provides essential nutrients directly into the bloodstream for patients who are unable to eat or digest food properly. While it can be lifesaving for individuals with severe malnutrition or gastrointestinal disorders. It requires careful monitoring and management to ensure safety and effectiveness.